[ad_1]
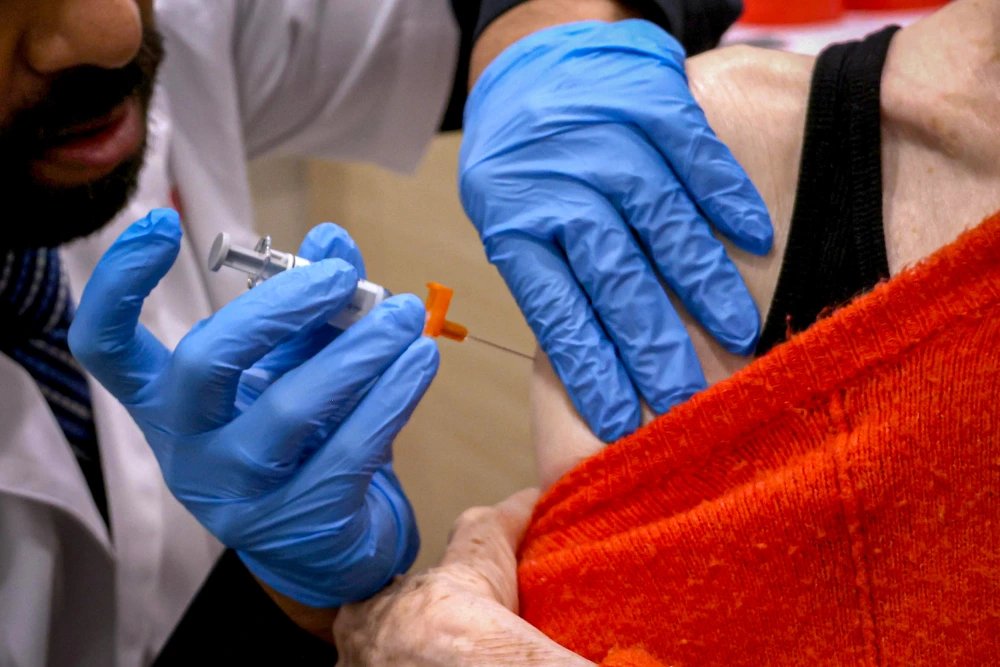
In October, the Centers for Disease Control and Prevention recommended that high-risk adults receive a second dose of the latest coronavirus vaccine for added protection against the virus.
Officials now recommend people 65 and older and those with weakened immune systems receive a second dose of the 2024-25 vaccine six months after the first dose, NBC News reports. I am doing it.
This is not the first time the agency has recommended or authorized additional doses for at-risk groups months after the first. In spring 2022, authorities approved a second booster shot after an initial fall rollout. The same pattern continued in spring 2023 and spring 2024.
No other vaccine is given as frequently, but experts say there is no reason to believe these vaccines, especially the mRNA vaccines from Pfizer and Moderna, are ineffective.
The Pfizer and Moderna vaccines are the first to use mRNA technology to induce immunity against the virus, an approach that is important at the beginning of the pandemic because mRNA vaccines can be developed much faster than traditional vaccines. It turned out that.
Despite the CDC’s recommendation for booster shots, there is no evidence that mRNA vaccines are not working as well as expected, said Akiko Iwasaki, a professor of immunology at Yale School of Medicine.
Rather, something specific to the virus may be preventing people’s bodies from maintaining high levels of immunity, Iwasaki says.
A recent study by researchers at Emory University found that so-called hybrid immunity (when a person has had both a vaccination and a coronavirus infection at some point) significantly reduces certain long-lasting cells that secrete antibodies. It turned out that it could not be established. Iwasaki said this is not the case for people who have received influenza or tetanus shots, suggesting something different is happening with the virus.
“You would think this kind of hybrid immunity would be the most stringent, but we still didn’t see this increase in the number of long-lived plasma cells,” she says.
Dr. Ashish Jha, dean of Brown University’s School of Public Health and former White House COVID-19 response coordinator, said there is some uncertainty about the durability of mRNA vaccines when compared to older vaccine technologies. said.
“It might be a little less durable,” Jha says. “I don’t think we know.”
The bigger problem, Jha said, is how quickly the virus mutates and is present year-round.
“The issue in my mind is more about the virus than the vaccine,” he said, adding that he supports the latest guidance.
“This is something I’ve actually encouraged my own parents to do, and it’s something I’ve said publicly,” he said.
The guidelines were announced amid concerns that weakened vaccination immunity, especially among older people, could make them more likely to develop severe illness and be hospitalized.
“It’s not a bad idea to boost immunity from vaccines every six to 12 months,” said E. John Wherry, an immunologist at the University of Pennsylvania. It added that the vaccine increases antibody levels, which are the first line of defense against the virus.
“This allows the remaining immune system to easily cleanse itself and prevent small illnesses that cause infections,” Wherry says.
A rapidly changing virus
“Every year we look at the strains of the influenza vaccine and try to match them as closely as possible,” said Dr. Anna Durbin, an infectious disease physician and associate professor at Johns Hopkins University School of Medicine. “COVID-19 has accelerated change even further, and we are constantly changing to gain an advantage.”
One reason booster shots for viruses like measles aren’t given as often is because viruses don’t change as quickly as coronaviruses.
“The measles virus you encounter today is very similar to the measles virus you might have encountered five or 10 years ago,” Jha says.
In an ideal world, coronavirus vaccines would be able to be updated more quickly to match the strains in circulation.
“By the time we choose which strain to switch to, and by the time the vaccine is ready and rolled out, some of the virus has already mutated,” Durkin said. “So the real question is, can we boost immunity that may not be fully compatible with the strains that are circulating?”
She said high-risk people could be better protected if immunity was strengthened by another vaccination.
Jha doesn’t expect twice-yearly vaccines to be universally recommended for all age groups, since a 30-year-old’s immune system is much stronger than an 80-year-old’s.
“Unless the virus becomes more virulent,” he said. “I don’t think that’s really going to happen.”
This article first appeared on NBCNews.com. More from NBC News:
[ad_2]Source link